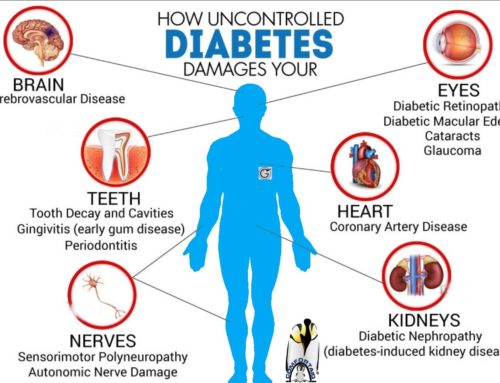
Diabetics are prone to Foot Infections due to a number of reasons:
- High blood sugar has adverse effects on cells throughout the body. One of the cell it effects is that of the immune system particularly cells that fight off bacteria. One such cell is called macrophage, which is a large call that eats up bacteria. When you have diabetes, these macrophages don’t function like they should and the bacteria can easily set up an infection in the body.
- Poor blood circulation in diabetics limits the access of these already malfunctioning immune cells to the infected area. Circulatory problems also result in poor antibiotic concentration in the infected area.
- Another problem with diabetes is that diabetics tend to get infection by more than just one or two different types of bacteria. Often times, diabetic foot infections have multiple different organisms in there. This further makes it difficult for the body to fight off different organisms at the same time.
- Our skin is a natural barrier that protects against bacterial invasion. One problem in diabetics is that wounds don’t heal very quickly resulting in loss of this skin barrier. This gives bacteria a much higher chance of setting up an infection in the body.
How can I help prevent foot infections?
Most common cause of diabetic foot infection is a foot ulcer. As mentioned in previous articles, foot care routine, do’s and don’ts of diabetic foot and daily foot self-exams are the cornerstone for preventing diabetic foot infections and other complications.
Different types of Diabetic Foot infections:
Diabetic foot infections can be broadly divided into fungal and bacterial. Let’s discuss them one by one.
1.0 Fungal Infections:
Fungal infection in diabetics most commonly involves the feet or toe nails. Although everyone carries fungi in their skin and under the nail edges, they don’t give complaints in most people. Diabetics are more prone to fungal infections due to reasons mentioned above. An infection can only occur when the fungi penetrate through the skin or nail.
- If it infects the toe nails, it’s called Onychomycosis.
- If it infects the skin, it’s called Athlete’s foot or Tinea Pedis.
Risk factors:
Fungal infection can easily spread to other people through skin flakes. You can also infect yourself, it usually starts on one toe and if untreated can spread to other toes as well. Or it starts as Athlete’s foot and then travels towards your toe nails
- Warm and humid environment
- Perspiring feet
- Badly ventilation socks and shoes
- Damaged nails
- Swimming and frequent showering- makes the skin moist and thus more prone to infection.
1.1 Onychomycosis/Toe nail fungus
Onychomycosis is extremely common but very stubborn to treatment. Reason being the organism that causes toe nail fungus doesn’t actually infect the nail tissue itself. It basically infects the skin under the toenail and uses the overlying nail as a shield under which it grows and spreads. This overlying nail acting as a shield makes it very difficult for topical antifungal cream/ointment to penetrate through.
Signs of onychomycosis
- Yellow nails with white streaks going across them
- Yellow-brown in later stages
- Brittle nails that chip easily around the edges
- Thick and uneven nail- The thickness makes the nail grow into your skin giving you ingrown toenails
- Itching
- Pain
IMPORTANT ADVICE
- The key to treating toe nail fungus quickly is to see your doctor as soon as you notice the symptoms.
- Your doctor will prescribe an oral anti-fungal medication which enter your bloodstream and work from the inside. You’ll have to take this medicine for a minimum of three months. It is very crucial that you take it regularly. Don’t even skip a day.
- If the nail is damaged severely, it can last up to a year after treatment before the new healthy nail is fully grown.
- Many people go for home-remedies route common ones being tea tree oil, apple cider vinegar, Listerine mouth wash etc. It is important that your talk with your healthcare provider before using any of these.
1.2 Athlete’s foot/Tinea pedis
It’s a fungal infection occurring between the toes and bottom of the feet. Very common condition but unlike toenail fungus, it’s very responsive to treatment. The fungus thrives in the warm and moist environment between your toes.
Signs of Athlete’s foot
- Peeling of skin between the toes
- Itching/Burning sensation
- Redness
- Foot odor
IMPORTANT ADVICE
- It is important to treat Athlete’s foot because the infection can spread to nails causing the more serious and resistant toenail fungal infection.
- Also it’s a very contagious condition and can be passed easily from one person to another. Do not share your items of personal hygiene with anyone.
- Most of the times, Athlete’s foot can be treated with over the counter anti-fungal creams/ointments. Your healthcare provider may also give prescription anti-fungal ointments and rarely oral medications if it’s resistant.
2.0 Bacterial Infections:
Bacterial infections in a diabetic can deteriorate very quickly and easily spread through out the foot. So it is extremely important for you to recognize signs and symptoms of infection and if you notice any of these, call your doctor RIGHT AWAY.
- Red streaks extending up the foot or leg
- Increased pain in your ankle
- Foul odor
- Grey or black tissue around the wound
- Wound getting larger
- Redness, swelling and increased warmth around the wound
- Wound drainage becomes bloody, green/yellow/brown drainage or there is increased clear drainage
- Pain/tenderness/redness/swelling/pus along the side of nail- sign of infected ingrown toenail.
- Pus discharge
- Delayed healing
- Soft or mushy tissue
- Fever/Chills- indicates a deep and severe infection
- Bone visible in the wound
Different Types of Bacterial Foot Infections:
2.1 Infected ingrown toe nail
A nail becomes ingrown when it grows into the skin. Cutting nails too short and wearing poorly fitted shoes increases the chance of developing ingrown toenails in diabetics. Ingrown toe nails have a very high chance of getting infected.
IMPORTANT ADVICE:
- As a diabetic, it is extremely important for you to see your healthcare provider as soon as possible. If untreated, the infection can easily and quickly spread to the rest of your foot including bone causing serious complications. Your doctor will take measures to release that infection by removing a portion of your nail. Most of the time the entire nail does not have to be removed.
- Some diabetics, even before consulting a doctor, apply very heavy antibacterial ointments on the toe if they suspect it’s infected. Most people think that applying such ointment to an infected toe nail is a good thing, it’s NOT. What happens is that the ointment acts like a barrier, compressing the infection inside as opposed to allowing it to come out. Best thing to do is see a podiatrist right away.
- NEVER perform bathroom surgery on your ingrown toenail. Leave it to the specialists.
- Bottom-line: Don’t mess with an ingrown toenail.
2.2 Cellulitis
Cellulitis is a bacterial infection of the skin and tissue immediately underneath it. Diabetics are very susceptible to developing cellulitis if minor injuries and cuts are not managed properly. Cellulitis is not a contagious infection.
2.3 Deep soft tissue infections
Infection in a diabetic can quickly spread into deeper tissues involving muscle (called Myositis), tendons (Tendonitis) and form abscess (pockets of pus).
2.4 Necrotizing Fasciitis
Also know as flesh eating bacteria. As the name suggests, it’s a condition that damages skin, muscles, fat and deeper tissues within a very short time. It’s a very serious and life-threatening condition that requires immediate emergency management. Necrotizing Fasciitis usually occurs after minor injury and starts as swelling and redness of the area. But the condition quickly deteriorates and the infection spreads within 24 hours. That’s why it’s extremely important for you to contact your healthcare provider as soon as you notice any of the symptoms mentioned above.
2.5 Osteomyelitis
Infection of the bone is called Osteomyelitis. Palpable bone during probing is suggestive of Ostermyelitis. Once infection spreads to the bone, you’ll need hospitalization for workup and management. Your health care provider may perform different tests to confirm the diagnosis. Your healthcare provide may take X-rays of your foot, perform bone scans or do a bone biopsy.
Management of Infections:
Determine Severity of Infection:
Your healthcare provider will determine the severity of your infection classifying it as mild, moderate or severe. This helps determine the appropriate antibiotic regimen, need for hospitalization or surgical intervention.
Obtaining Cultures:
- Your healthcare provider will take deep tissue cultures from the infected area to see what type of infection you have, which organisms are involved and which antibiotics will work best.
- Antibiotics will be immediately started after obtaining cultures and modified accordingly when result of culture and sensitivity become available.
Taking Antibiotics:
- Mild to moderate infection is managed in an outpatient setting. Your healthcare provider will prescribe oral antibiotics for 4-6 weeks. Finish you antibiotics as advised by your doctor. Do not skip doses.
- Severe infections need hospitalization and intravenous antibiotics.
Debridement:
See article on diabetic foot ulcers (Release date July 26th, 2013)
Wound management:
Appropriate dressing and off-loading (See article on diabetic foot ulcers).
Metabolic Stability:
- Eat a healthy and balanced diet as advised by your doctor.
- Maintain your blood glucose in target range.
- Keep your blood pressure and cholesterol under control.
- Don’t smoke
Important Note:
Diabetes and Foot Care … read more:
- Diabetes and Alcohol Consumption – Latest Release





Leave A Comment