Type 1 diabetes is a disorder characterized by abnormally high blood sugar levels. In this form of diabetes, specialized cells in the pancreas called beta cells stop producing insulin. Insulin controls how much glucose (a type of sugar) is passed from the blood into cells for conversion to energy. Lack of insulin results in the inability to use glucose for energy or to control the amount of sugar in the blood.
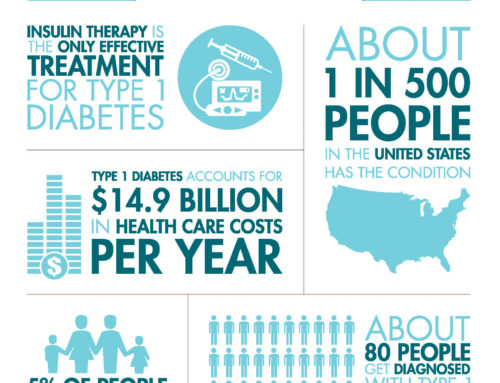
Type 1 diabetes is usually diagnosed in children and young adults, and was previously known as juvenile diabetes. Only 5% of people with diabetes have this form of the disease. In the United States, the peak age at diagnosis is around 14.
Type 1 diabetes can occur at any age; however, it usually develops by early adulthood, most often starting in adolescence. The first signs and symptoms of the disorder are caused by high blood sugar and may include frequent urination (polyuria), excessive thirst (polydipsia), fatigue, blurred vision, tingling or loss of feeling in the hands and feet, and weight loss.
It has been estimated that the yearly incidence of type 1 diabetes developing is at most 0.02%(percent). However, more than 700,000 Americans have this type of diabetes. This is about 10% of all the Americans diagnosed with diabetes; the other 90% have type 2 diabetes.
In type 1 diabetes, the body does not produce insulin. The body breaks down the sugars and starches you eat into a simple sugar called glucose, which it uses for energy. Insulin is a hormone that the body needs to get glucose from the bloodstream into the cells of the body. With the help of insulin therapy and other treatments, even young children can learn to manage their condition and live long, healthy lives.
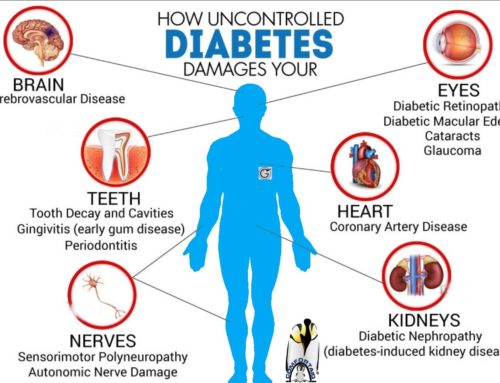
These symptoms may recur during the course of the disorder if blood sugar is not well controlled by insulin replacement therapy. Improper control can also cause blood sugar levels to become too low (hypoglycemia). This may occur when the body’s needs change, such as during exercise or if eating is delayed. Hypoglycemia can cause headache, dizziness, hunger, shaking, sweating, weakness, and agitation.
Uncontrolled type 1 diabetes can lead to a life-threatening complication called diabetic ketoacidosis. Without insulin, cells cannot take in glucose. A lack of glucose in cells prompts the liver to try to compensate by releasing more glucose into the blood, and blood sugar can become extremely high. The cells, unable to use the glucose in the blood for energy, respond by using fats instead. Breaking down fats to obtain energy produces waste products called ketones, which can build up to toxic levels in people with type 1 diabetes, resulting in diabetic ketoacidosis. Affected individuals may begin breathing rapidly; develop a fruity odor in the breath; and experience nausea, vomiting, facial flushing, stomach pain, and dryness of the mouth (xerostomia). In severe cases, diabetic ketoacidosis can lead to coma and death.
5. How is Juvenile Diabetes diagnosed?
What tests are used to diagnose diabetes in children?
If your child has symptoms of diabetes, or if you think they may be at-risk for developing diabetes, they should be tested for the disease.
- A glucometer: A hand-held device that tests your blood sugar levels using a small drop of blood from the tip of the finger
- A urine sample: A simple urine collection that your doctor will use to test for the presence of sugar in the urine
o For type 1 diabetes, it’s important to evaluate the acid levels in blood and urine. - An oral glucose tolerance test (OGTT): A test that’s similar to what doctors do to test for diabetes during pregnancy that tests for type 2 diabetes
- Hemoglobin A1c: This blood test looks for chronic elevations in blood sugar in kids with type 1 or type 2 diabetes.
How do doctors at Children’s Hospital diagnose and treat diabetes?
Children who are admitted to the emergency department and exhibit signs and symptoms of diabetes will be evaluated for their condition. The doctors will perform blood tests to evaluate the levels of sugar and acid in the blood.
If these levels are only mildly elevated, your child may receive fluids through an IV(ivey), followed by one to two injections of insulin. The next day, doctors may recommend families to visit Centre for Childhood Diabetes in their neighbourhoods for education and training on how to manage new diabetes.
However, if a child’s blood sugar and acid levels are very high, the doctors will provide fluids and insulin through an IV(ivey) and admit them to the hospital for one or two days. The day after discharge, doctors may recommend the family to visit the A Center for New Diabetes education.
Most children with newly diagnosed type 1 diabetes are not acutely ill. Families generally come to the Center within a few weeks of diagnosis for education specifically designed for children with type 1 diabetes.
If your primary care provider thinks your child may have type 2 diabetes, you may be referred to the Children’s Hospital. At the Children Hospital, a multidisciplinary team of pediatric experts will conduct a comprehensive medical assessment to provide the specialized treatment your child needs.
Managing juvenile diabetes is a difficult task. As a parent, Parent(s)need as much help as Parent(s)can get. Education is also very helpful in managing this condition. To find more information about juvenile diabetes, how to cope, and how to get involved with other parents, consult the following links.


Leave A Comment